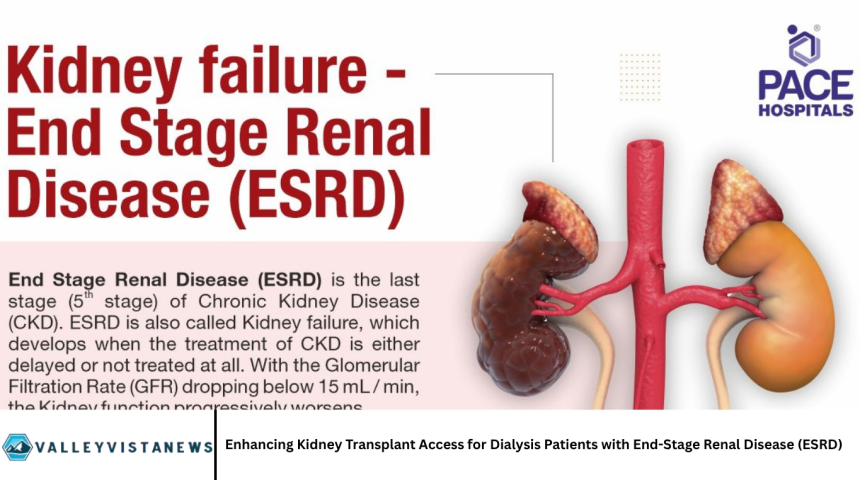
End-Stage Renal Disease (ESRD) is the final, most severe stage of chronic kidney disease (CKD), characterized by the irreversible loss of kidney function. For patients with ESRD, dialysis and kidney transplantation are the two primary treatment modalities that sustain life.
While dialysis serves as a life-saving interim therapy, kidney transplantation remains the gold standard treatment, offering better survival rates, improved quality of life, and lower long-term healthcare costs.
Despite these benefits, many dialysis patients face barriers to accessing kidney transplantation. This article explores the current landscape of kidney transplantation access for dialysis patients with ESRD, identifies challenges, discusses ongoing efforts to enhance access, and outlines potential strategies to improve transplantation rates and outcomes.
Understanding End-Stage Renal Disease (ESRD)
ESRD occurs when kidneys lose approximately 85-90% of their function, making it impossible to sustain life without renal replacement therapy (RRT) such as dialysis or transplantation. Causes include diabetes, hypertension, glomerulonephritis, and other chronic conditions.
Patients with ESRD experience complications including fluid overload, electrolyte imbalance, anemia, bone disease, cardiovascular problems, and diminished quality of life. Managing ESRD requires a multidisciplinary approach, including nephrologists, transplant surgeons, dietitians, social workers, and other healthcare providers.
Dialysis: A Life-Sustaining but Imperfect Solution
Dialysis substitutes for lost kidney function by removing waste products and excess fluids from the blood. There are two main types:
- Hemodialysis: Blood is filtered through a machine, typically done in a clinic multiple times per week.
- Peritoneal Dialysis: Utilizes the patient’s peritoneum as a filter, performed at home.
While dialysis extends life, it is associated with significant limitations:
- Increased risk of infections and cardiovascular complications.
- Reduced quality of life due to frequent treatments and dietary restrictions.
- High healthcare costs and resource utilization.
Kidney Transplantation: The Preferred Treatment for ESRD
Kidney transplantation involves replacing a failed kidney with a healthy one from a living or deceased donor. It offers numerous advantages over dialysis:
- Improved Survival: Transplant recipients live significantly longer than patients remaining on dialysis.
- Better Quality of Life: Freedom from dialysis sessions and dietary restrictions enhances daily living.
- Cost-effectiveness: Though upfront costs are high, transplantation reduces long-term healthcare spending.
Despite these benefits, kidney transplantation is not universally accessible to all eligible patients.
Barriers to Kidney Transplant Access for Dialysis Patients
Organ Shortage
One of the most pressing challenges is the chronic shortage of donor kidneys. Demand far exceeds supply, leading to long waiting times, sometimes spanning several years.
Inequities in Referral and Evaluation
Not all dialysis patients are referred timely for transplant evaluation. Racial and socioeconomic disparities affect referral rates, with minority groups often disadvantaged.
Medical Contraindications
Certain comorbid conditions, such as active infections, cancer, or severe cardiovascular disease, can preclude transplantation candidacy.
Psychosocial Barriers
Mental health disorders, lack of social support, or substance abuse history can affect eligibility or complicate post-transplant care.
Geographic and Institutional Factors
Access varies by location and healthcare system, with rural patients and those in under-resourced centers facing greater challenges.
Current Efforts to Improve Access to Kidney Transplantation
Policy and Regulatory Changes
- Kidney Allocation System (KAS): Revised to improve equity by prioritizing candidates based on factors like time on dialysis and sensitization.
- Living Donor Programs: Expansion and promotion to increase kidney availability.
Patient Education and Outreach
Programs to raise awareness about transplantation benefits and encourage early referral are increasingly adopted.
Telemedicine and Remote Evaluation
Telehealth platforms enable pre-transplant evaluations and consultations, reducing geographic barriers.
Research and Innovation
Studies focusing on desensitization protocols, paired kidney exchanges, and xenotransplantation hold promise for expanding donor pools.
Strategies to Further Enhance Transplant Access
Increasing Organ Donation Rates
- Public education campaigns.
- Opt-out donation policies.
- Incentivizing donation through ethical means.
Improving Pre-Transplant Care
- Early nephrology referral.
- Optimizing comorbidities.
- Mental health support.
Enhancing Post-Transplant Support
- Adherence counseling.
- Regular follow-up.
- Addressing socioeconomic challenges.
The Role of Healthcare Providers and Systems
Healthcare teams play a critical role in identifying transplant candidates, facilitating evaluations, and supporting patients through the process. Collaboration across nephrology, transplant surgery, nursing, social work, and pharmacy is essential.
Systems-level interventions, such as standardized referral protocols and quality improvement initiatives, have demonstrated success in improving transplant access.
Patient Perspectives and Experiences
Understanding patient views is vital. Common concerns include fears about surgery, uncertainty about organ availability, financial worries, and trust in the healthcare system.
Peer support groups, patient navigators, and counseling services help address these issues.
Future Directions
Emerging technologies such as artificial intelligence may optimize donor-recipient matching. Advances in immunosuppression aim to reduce rejection and improve graft longevity. Continued advocacy for organ donation and equitable healthcare policies remain paramount.
Frequently Asked Questions
Why is kidney transplantation preferred over dialysis for ESRD patients?
Transplantation offers better survival rates, improved quality of life, and lower long-term costs compared to dialysis.
What factors limit access to kidney transplantation?
Organ shortages, medical contraindications, socioeconomic disparities, and geographic barriers all limit access.
How long is the typical wait time for a kidney transplant?
Wait times vary but often range from 3 to 7 years depending on blood type, sensitization, and geographic location.
Can living donors increase transplant availability?
Yes, living donor transplants reduce wait times and often yield better outcomes than deceased donor kidneys.
What role do socioeconomic factors play in transplant access?
They affect referral rates, evaluation completion, and ability to afford medications and follow-up care.
How can patients improve their chances of getting a transplant?
Early referral, managing health conditions, adhering to treatment, and seeking living donors can help.
Are there new technologies to address organ shortages?
Research on paired exchanges, desensitization, and xenotransplantation shows promise for expanding donor pools.
Conclusion
Enhancing kidney transplant access for dialysis patients with ESRD requires a multifaceted approach addressing organ shortage, systemic inequities, medical and psychosocial barriers, and patient education. Improving access promises to save lives, improve quality of life, and reduce healthcare costs. Continued commitment from policymakers, healthcare providers, patients, and communities is crucial to realizing this goal.