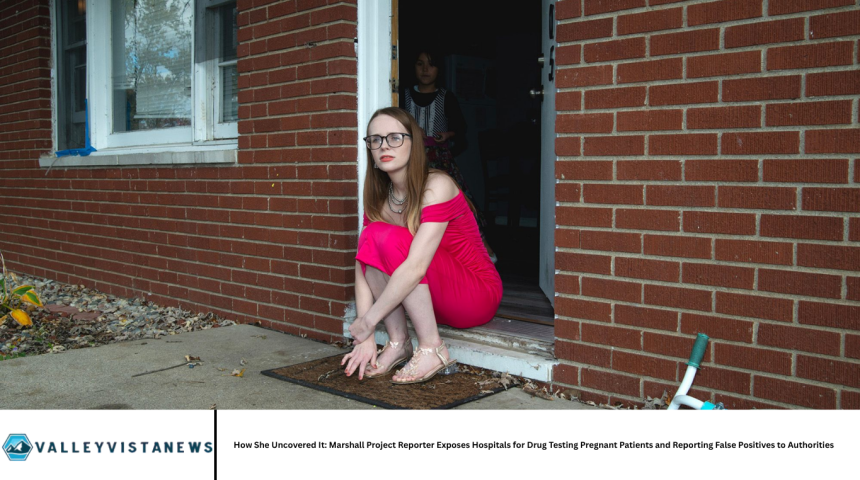
Shoshana Walter, a veteran investigative reporter at The Marshall Project, embarked on a deeply troubling investigation: hospitals across the U.S. were testing pregnant and laboring women for drugs, often without consent, and reporting positive results to child welfare agencies—even when those results were false and caused by medications administered in childbirth.
Her reporting revealed systemic failings, racial disparities, and a lack of due process. This article traces her investigative process, depicts personal stories from affected women, analyzes systemic issues, highlights legal and ethical implications, and outlines reform proposals to ensure that mothers and infants are protected.
Launching the Investigation: Piecing Together a Hidden Crisis
Walter began with a simple observation: hospitals were drug-testing laboring patients and reporting them to child protective services, yet there was no public dataset tracking how often or where this occurred. To build her understanding, she conducted dozens of interviews—with women subjected to testing, medical professionals, social workers, toxicologists, and legal experts. She combed through medical records, court filings, and state-level policies mandating drug-exposed infant reporting. By connecting patterns across states and institutions, Walter demonstrated that these were not isolated incidents but widespread and structurally rooted practices that disproportionately impacted marginalized communities.
The Mechanics of False Positives: Medications Mistaken for Illicit Substances
One of Walter’s key discoveries was that routine labor treatments often triggered false positive screens. Standard hospital drug tests—immunoassay urine tests—lack specificity and are sensitive to legally prescribed medications:
- Fentanyl and morphine, administered during labor or epidural, can register as positive for illegal opioids.
- Benzodiazepines like midazolam, given for sedation, often produce positive screens without illicit intake.
- Blood pressure medications used during surgery—such as phenylephrine or ephedrine—have been linked to methamphetamine false positives.
- Even poppy seeds, consumed in normal foods, and the over-the-counter antacid ranitidine, have triggered opioid positives.
Because hospital protocols in many states require reporting based solely on these initial tests, mothers found themselves under investigation despite no illicit drug use.
Stories of Harm: Lives Turned Upside Down
Walter shared the stories of several women who experienced trauma as a result:
- A woman in Indiana who received morphine during labor later learned she tested positive for opioids. Although the medications were administered by medical staff, she feared she’d lose custody of her child.
- A Texas mother who suffered a stillbirth and underwent emergency surgery was sedated with midazolam. Hospital staff reported a drug-positive result despite no illicit drug use. She endured months of investigation before being cleared, all while grieving and separated from her newborn.
- In Oklahoma, a mother taking common heartburn medication tested positive for methamphetamine and her four children were placed into foster care temporarily until the error was confirmed.
Across dozens of cases, Walter documented common patterns: women were frequently tested without consent, positive results came from hospital-administered medications, and hospitals reported them without confirmatory testing. Investigations upended births, caused prolonged stress, and in many cases, led to temporary separation of mother and child.
Systemic Failings: Mandatory Policies, Lack of Consent, and Disproportionate Impact
Mandatory Reporting Laws
In more than two dozen U.S. states, law requires hospitals to report any drug-exposed newborn or mother—even without medicinal context or confirmatory tests. These laws shield providers from liability when making reports but do not require accuracy or medical judgment.
Absence of Informed Consent
Most pregnant patients reported they were unaware they were being drug-tested. Hospitals rarely provide written consent forms, and testing is often embedded in routine panels without explanation or opt-out options.
Racial and Economic Disparities
Walter’s investigation found that Black, Indigenous, Latinx, and low-income women face significantly higher rates of testing and reporting. Investigations disproportionately target these groups, even when confirmatory tests later show no illicit drug use.
Institutional Pressures
Hospital staff often operate under heavy workloads and limited guidance. Social workers, midwives, or nurses may follow outdated protocols or fear personal liability, leading to deterministic decisions rather than nuanced clinical judgments.
Legal and Ethical Implications
Constitutional Protections
A 2001 Supreme Court ruling declared involuntary drug testing of pregnant women, without consent or medical justification, unconstitutional. Despite this, many hospitals continue such practices under the guise of neonatal protection.
Civil Rights Violations
Ongoing litigation in states like New York, New Jersey, and Vermont alleges that drug-testing policies violate patient privacy and civil rights laws. These cases argue that hospitals and state agencies have failed to protect mothers’ rights.
Medical Ethics and Trust
The practice erodes trust in hospitals among birthing people—especially women of color—undermining prenatal care engagement and public health outreach. Medical ethics emphasize informed consent, accurate testing, and non-maleficence, all of which these protocols violate.
Reform Recommendations
Hospital Policy Reforms
Some systems have changed practices: they no longer test for drugs without consent or a valid clinical indication, and they avoid automatic reporting. Confirmatory lab testing is required before initiating a CPS report.
Legislative and Regulatory Changes
Reform advocates urge changes such as:
- Mandatory confirmatory testing before any reporting.
- Consent required before drug tests are performed.
- Exemptions for hospital-administered medications.
- Removal of blanket reporting statutes in favor of clinical discretion.
Community and Patient Advocacy
Pregnant patients are encouraged to ask questions, seek second opinions, share experiences, and demand transparency. Grassroots legal and advocacy groups, like Pregnancy Justice and the ACLU, play key roles in pushing for accountability and policy change.
The Power of Investigative Journalism
Walter’s approach underscores that absence of centralized data shouldn’t prevent uncovering systemic injustice. By gathering qualitative evidence—survivor stories, medical records, state statutes, interviews—we can construct a compelling case for change. She demonstrated how narrative evidence and persistent inquiry can lead to impactful reporting and public policy reform.
Frequently Asked Questions
Can hospitals drug-test pregnant patients without their consent?
In many cases, yes—with testing often embedded in routine hospital protocols. That practice conflicts with U.S. Supreme Court precedent protecting against involuntary testing.
How do legal medications cause false-positive drug tests?
Common medications given during labor—opioids, sedatives, blood pressure drugs—and even foods like poppy seeds can trigger immunoassays used in hospitals, which lack specificity.
What harm results from false positive tests?
Mothers can be reported to child services, subjected to investigations, separated from newborns, and endure emotional trauma—even when there is no illicit substance use.
Why don’t hospitals wait for confirmatory testing before reporting?
Many state laws mandate reporting even on screening results. Confirmatory testing is not legally required and hospitals often lack incentives to delay reporting.
Who is most impacted by this system?
Black, Indigenous, Latinx, and low-income women are disproportionately tested, investigated, and less likely to reunify with their infants after separation.
What legal protections exist for affected mothers?
The 2001 Supreme Court ruling prohibits nonconsensual testing tied to law enforcement. Some states are passing or considering laws requiring consent and confirmatory testing. Civil rights lawsuits are ongoing.
How can the situation be improved?
Reforms include: requiring informed consent, imposing confirmatory test mandates, allowing clinical judgment before reporting, removing mandatory reporting triggers, and improving provider training on maternal rights.
Conclusion
Shoshana Walter’s investigation revealed a deeply entrenched practice within many U.S. hospitals—drug testing pregnant patients without consent and reporting false positives that stem from administered medications. These reports have resulted in unnecessary tears, investigations, and separations, disproportionately harming marginalized women. Her reporting has catalyzed policy reevaluation, ongoing litigation, and broad calls for change. For public health and reproductive justice to advance, transparency, consent, and accuracy must replace fear-based protocols.